Prevention of Cervical Cancer in India through Self Sampling
Toronto Metropolitan University
A mother living in the State of Maharashtra, India, Meera was reluctant to have herself and her daughters screened for cervical cancer when the opportunity was presented. Although her region has a high prevalence of cervical cancer, Meera and many other women believed that only women who have a ‘loose character’ could be diagnosed.
Meera’s limited knowledge about cervical cancer and sexually transmitted infections (STIs) was putting her and her family at risk. Her village has a very high prevalence of cervical cancer, high-risk behaviours, and low uptake of cervical cancer screening. This can be attributed to factors such as limited knowledge and awareness, difficulty in accessing services, cultural barriers such as modesty, and stigma surrounding STIs such as HPV (the primary cause of cervical cancer). Entrenched gender norms and stereotypes associated with STIs in India are the major deterrents to screening uptake.

The high incidence rate in Meera’s village is consistent with national statistics in India, where cervical cancer is the second leading cause of deaths preventable through regular screenings. In many high-income nations, the incidence and mortality of cervical cancer has declined substantially because of the widespread use of Pap tests as a screening tool, however, the coverage of cervical cancer screening in developing countries like India is only 19% (compared to 63% in developed countries).
Supported by FIT, Toronto Metropolitan University and Tata Memorial Hospital tested an innovative solution that aimed to promote cervical cancer screening through HPV self-sampling (HPV-SS) and involved a family-centered approach that engaged both men and women. The HPV-SS is an easy and user-friendly alternative to the costly, traditional modalities of cancer screening and has been found to be effective in engaging under and never screened (UNS) women. The approach promoted open dialogue between men and women around gender equity, in order to ensure that women had the support of their male partners when it came to cervical screening. After the screenings, women were provided access to further medical support and follow-up in an effort to improve long term health outcomes for women in the region.
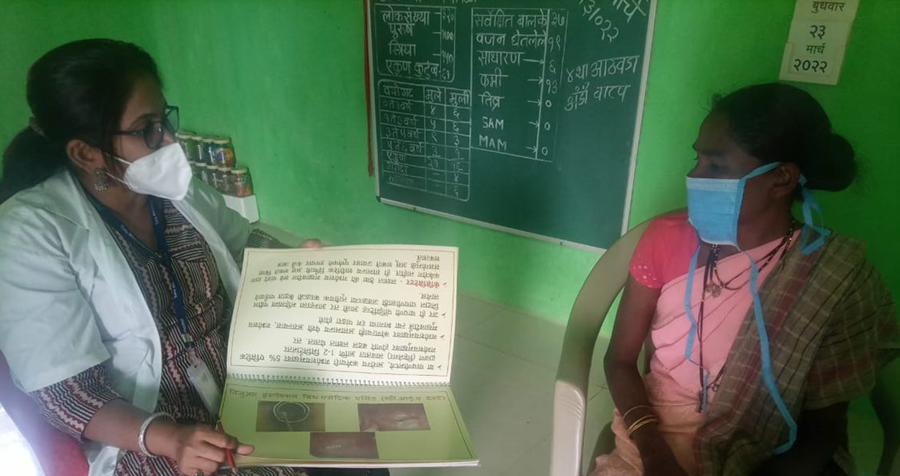
This was supplemented by an art-based and culturally appropriate sexual health literacy intervention. Key to the dissemination of knowledge was the use of visual aids such as detailed pictures, infographics, and movies to convey information in a way that was engaging and easy to understand (especially for participants who had difficulty reading). The innovation also engaged community health care volunteers, known as ASHA, to promote cervical cancer screening uptake among local populations.

Results indicated a significant increase in knowledge, positive attitudes towards cervical cancer screening, and a significant reduction in stigma surrounding STIs among participants who attended the sexual health education (SHE) sessions. Using a gender lens was crucial to destigmatizing both STI and cervical cancer and ensuring that men were also aware of the benefits of screening. The involvement of men as supportive partners was also essential in promoting open dialogue between family members to reduce victim blaming. The innovation also successfully trained 451 local workers to raise awareness about cervical cancer and promote the HPV-SS test in their communities.
Since participating in the innovation, Meera and her husband have changed their attitudes towards STIs and recognize the importance of screening for HPV in the early detection of cervical cancer. They now know that nobody should feel ashamed, and that catching it early results in better health outcomes for women. This knowledge is crucial for destigmatizing STIs and promoting life-saving screenings among communities in the region. With the knowledge gained through PCCIS, Meera and her husband are now encouraging their daughters and sisters to go for screenings as well.
“As some women might not understand what this test is about…we would first convince the family members, involve them, make them understand the importance of this test, also share our experiences with them and make them aware that it is a safe test.
We shall give women some space to think (think for themselves about the importance of tests). We can support them by giving them company at the camp.”
- Tata Memorial Hospital staff person


